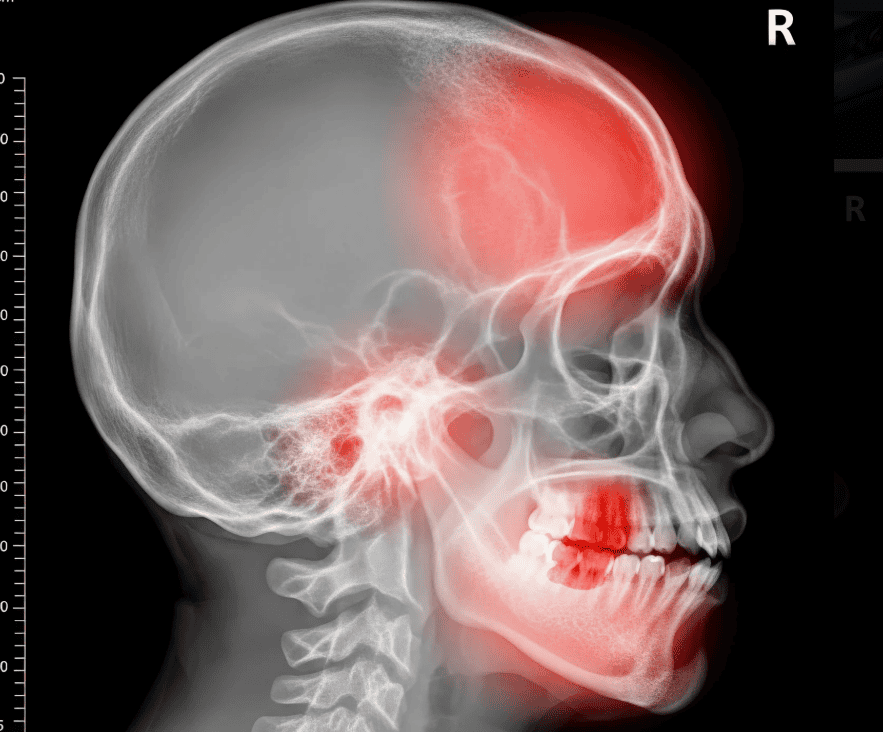
When facing a serious medical condition, most patients begin their journey with conventional, FDA-approved treatments that have demonstrated safety and efficacy through rigorous clinical trials. However, for some individuals, these standard options prove ineffective or unsuitable due to contraindications, side effects, or disease progression.
Understanding what alternatives exist when conventional treatments fail can provide hope and potentially life-saving options for patients and their families.
The Reality of Treatment Failure
Medical science has made tremendous advances, yet standard treatments don’t work for everyone. Research indicates that approximately 30-40% of cancer patients do not respond adequately to first-line therapies, while in conditions like treatment-resistant depression, up to 30% of patients fail to achieve remission with conventional antidepressants. These statistics underscore a significant gap in healthcare affecting millions worldwide.
The reasons for treatment failure vary widely. Some patients develop resistance to medications over time, particularly common in cancer and infectious diseases.
Others experience severe adverse reactions that make continuing treatment impossible. Additionally, certain genetic variations can render standard therapies ineffective for specific individuals.

Expanded Access Programs
One of the most important resources for patients who have exhausted conventional options is expanded access programs, also known as compassionate use programs.
These initiatives allow patients with serious or life-threatening conditions to access investigational drugs that haven’t yet received full regulatory approval. According to Early Access Care (https://earlyaccesscare.com/services/post-trial-access), “post-trial access programs enable patients who have completed participation in clinical trials to continue receiving investigational treatments that showed promise.”
The FDA reports that it approves approximately 99% of expanded access requests, demonstrating a strong commitment to helping patients in need. However, awareness of these programs remains relatively low among both patients and healthcare providers.
In a survey of oncologists, fewer than 50% reported being familiar with the process of applying for expanded access, suggesting that many eligible patients may not be exploring this avenue.
Clinical Trial Participation
Clinical trials represent another crucial pathway for patients seeking alternatives when standard treatments have failed. These research studies test new therapies, drug combinations, or treatment approaches that may offer benefits beyond currently available options.
The National Institutes of Health maintains a database with over 400,000 registered clinical trials worldwide, many of which specifically recruit patients who haven’t responded to conventional therapies.
Participating in a clinical trial provides access to cutting-edge treatments years before they become widely available. Importantly, patients in clinical trials often receive closer monitoring and more comprehensive care than they would in standard treatment settings.
While there are no guarantees of efficacy and some patients may receive a placebo, many trials are designed to ensure all participants receive at least the standard of care, with the investigational treatment offered as an additional intervention.
Off-Label Drug Use
Off-label prescribing occurs when physicians use FDA-approved medications for purposes other than their officially approved indications. This practice is entirely legal and surprisingly common, accounting for approximately 20% of all prescriptions in the United States. In certain specialties like oncology and pediatrics, off-label use can represent more than 50% of prescriptions.
When conventional treatments fail, physicians may consider off-label options based on emerging research or mechanistic reasoning about how a drug might work for a particular condition.
While off-label use doesn’t undergo the same rigorous testing as approved indications, it can provide valuable alternatives when other options are unavailable.

Integrative and Supportive Approaches
Beyond pharmaceutical interventions, patients facing treatment failure should consider integrative approaches that support overall health and wellbeing. While not replacements for medical treatment, strategies like nutritional optimization, stress reduction techniques, and psychological support can improve quality of life and may enhance the effectiveness of other therapies.
Research increasingly supports the role of lifestyle factors in disease outcomes. Studies have shown that cancer patients who engage in regular physical activity during treatment experience better outcomes and fewer side effects. Mind-body interventions like meditation have also demonstrated benefits for pain management and treatment-related anxiety.
Advocating for Yourself
When conventional treatments fail, effective self-advocacy becomes essential. Patients should seek second opinions from specialists at major medical centers, particularly those affiliated with research institutions that may have access to novel therapies.
Connecting with patient advocacy organizations specific to one’s condition can provide valuable information about emerging treatments and access programs.
Documentation is crucial throughout this process. Maintaining comprehensive medical records, understanding one’s diagnosis and treatment history, and asking detailed questions about all available options empowers patients to make informed decisions.
Building a strong relationship with your healthcare team and clearly communicating your goals, concerns, and preferences ensures that everyone is working toward the same objectives.
When Conventional Treatments Fail – Moving Forward with Hope
The landscape of medical treatment continues to evolve rapidly, with new therapies emerging regularly. Advances in precision medicine, immunotherapy, and targeted treatments are expanding options for conditions that were previously difficult to treat.
For patients facing treatment failure, staying informed about developments and maintaining open communication with healthcare providers can reveal new possibilities.
While the journey can feel overwhelming, numerous resources and alternatives exist that may offer hope when standard approaches have been exhausted. Whether through expanded access programs, clinical trials, off-label use, or integrative approaches, patients today have more options than ever before.